Diabetes, or diabetes mellitus, is a condition where your blood sugar (glucose) levels are consistently higher than what’s considered normal. Why does this happen? Well, it boils down to two main reasons: either your pancreas isn’t producing enough insulin, or your body isn’t using the insulin it does produce effectively.
Insulin is a hormone that acts as a “key” to allow glucose from the food you eat to enter your cells and be used for energy. Without enough insulin or proper insulin function, that glucose ends up accumulating in your bloodstream, leading to high blood sugar levels.
The Different Types of Diabetes
Diabetes isn’t a one-size-fits-all condition – there are actually several different types, each with its own unique characteristics and causes. Let’s break them down!
Type 2 Diabetes
This is the most common form of diabetes, accounting for about 90-95% of all cases. In Type 2 diabetes, your body either doesn’t produce enough insulin or doesn’t use it effectively (a condition known as insulin resistance). This type primarily affects adults, but unfortunately, even kids aren’t immune.
Prediabetes
Think of prediabetes as a warning sign – your blood sugar levels are higher than normal, but not quite high enough to be classified as full-blown Type 2 diabetes. It’s a wake-up call to make some lifestyle changes before things progress further.
Type 1 Diabetes
Unlike its Type 2 counterpart, Type 1 diabetes is an autoimmune disease where your body’s immune system mistakenly attacks and destroys the insulin-producing cells in your pancreas. This type accounts for up to 10% of diabetes cases and is usually diagnosed in children and young adults, although it can develop at any age.
Gestational Diabetes
This type of diabetes develops during pregnancy and usually resolves after giving birth. However, if you’ve had gestational diabetes, you’re at a higher risk of developing Type 2 diabetes later in life, so it’s important to stay vigilant.

A Global Health Concern
Diabetes is more common than you might think. In the United States alone, approximately 37.3 million people (that’s about 11% of the population) are living with diabetes. Globally, the numbers are more staggering, with an estimated 537 million adults affected – a figure that’s expected to rise to a whopping 783 million by 2045.
Symptoms of Diabetes
While some types of diabetes, like Type 2 and prediabetes, can be asymptomatic (meaning they don’t show any obvious signs), others can present with a range of symptoms. Some of the most common symptoms to watch out for are increased thirst (polydipsia) and dry mouth, frequent urination, fatigue, blurred vision, unexplained weight loss, numbness or tingling in your hands or feet, slow-healing sores or cuts, and frequent skin and/or vaginal yeast infections.
In the case of Type 1 diabetes, symptoms can develop rapidly over a few weeks or months and can include additional signs like vomiting, stomach pains, fruity-smelling breath, and labored breathing – all indicators of a potentially life-threatening complication called diabetic ketoacidosis (DKA).
If you or a loved one experiences any of these symptoms, it’s crucial to seek medical attention right away.
Understanding the Root Causes of Diabetes
Now that we’ve covered the different types and symptoms, let’s dive into what actually causes diabetes in the first place.
Insulin Resistance
As mentioned earlier, insulin resistance is a major player in the development of Type 2 diabetes. This occurs when your cells become less responsive to insulin, preventing glucose from entering them effectively. Several factors can contribute to insulin resistance such as obesity, lack of physical activity, poor diet, hormonal imbalances, genetics, and certain medications.
Autoimmune Dysfunction in Type 1 Diabetes and LADA
In Type 1 diabetes and LADA (Latent Autoimmune Diabetes in Adults), the culprit is an autoimmune reaction where your body’s immune system mistakenly attacks and destroys the insulin-producing cells in your pancreas.
Hormonal Imbalances and Gestational Diabetes
During pregnancy, the placenta releases hormones that can cause insulin resistance. If your pancreas can’t compensate by producing enough insulin, you may develop gestational diabetes.
Pancreatic Damage and Type 3c Diabetes
Physical damage to your pancreas, whether from conditions like pancreatitis, pancreatic cancer, cystic fibrosis, or even surgery, can impair its ability to produce insulin, leading to Type 3c diabetes.
Genetic Mutations and Rare Forms of Diabetes
Certain genetic mutations can cause rare forms of diabetes like MODY (Maturity-Onset Diabetes of the Young) and neonatal diabetes, which affect insulin production or function from a very early age.
Medication Side Effects
Believe it or not, some medications can increase your risk of developing Type 2 diabetes as a side effect. These include certain HIV/AIDS medications and corticosteroids.

Complications of Diabetes
If left unmanaged, diabetes can lead to a host of sudden and long-term complications, primarily due to prolonged high blood sugar levels.
Acute Complications
Below are some of the sudden and severe outcomes if an individual doesn’t act on a known case of diabetes!
Hyperosmolar Hyperglycemic State (HHS)
This life-threatening complication, which mainly affects people with Type 2 diabetes, occurs when blood sugar levels are extremely high (over 600 mg/dL) for an extended period, leading to severe dehydration and confusion.
Diabetic Ketoacidosis (DKA)
As mentioned earlier, DKA is a potentially fatal complication that mainly affects people with Type 1 diabetes or undiagnosed Type 1. It occurs when your body doesn’t have enough insulin, forcing it to break down fat for energy instead, releasing acidic substances called ketones.
Severe Hypoglycemia (Low Blood Sugar)
This complication, which primarily affects people with diabetes who use insulin, occurs when blood sugar levels drop dangerously low, causing symptoms like blurred vision, disorientation, and seizures.

Long-Term Complications
Chronic high blood sugar can cause havoc on your body’s tissues and organs, primarily due to damage to your blood vessels and nerves. Some of the most common long-term complications include cardiovascular issues, nerve damage, kidney damage, eye damage, diabetes-related foot conditions, skin infections, amputations, sexual dysfunction, gastroparesis, hearing loss, and/or oral health issues.
Additionally, living with diabetes can take a toll on your mental health, as people with the condition are two to three times more likely to experience depression than those without it.
Diagnosing Diabetes
If your healthcare provider suspects you may have diabetes, they’ll likely order one or more of the following blood tests!
Fasting Blood Glucose Test
This test measures your baseline blood sugar levels after fasting (not eating or drinking anything except water) for at least eight hours.
Random Blood Glucose Test
As the name implies, this test can be done at any time, regardless of when you last ate.
A1C Test (Glycated Hemoglobin)
This test provides an average of your blood glucose levels over the past two to three months.

For gestational diabetes, your provider will order an oral glucose tolerance test.
Here’s a breakdown of the typical test result ranges!
| Test | In-Range (mg/dL) | Prediabetes (mg/dL) | Diabetes (mg/dL) |
| Fasting Blood Glucose | < 100 | 100 – 125 | ≥ 126 |
| Random Blood Glucose | N/A | N/A | ≥ 200 (with symptoms) |
| A1C | < 5.7% | 5.7% – 6.4% | ≥ 6.5% |
Managing Diabetes
Diabetes management is a complex and highly individualized process, but it typically involves a combination of the following strategies!
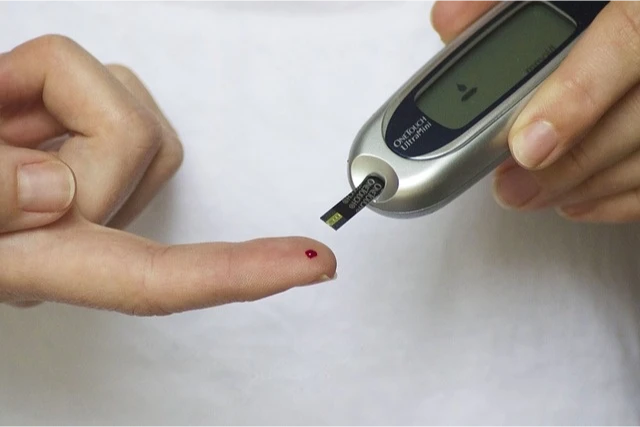
Blood Sugar Monitoring
Keeping a close eye on your blood sugar levels is crucial for determining how well your treatment plan is working and making any necessary adjustments. You can monitor your levels with:
- Frequent finger-prick tests using a glucose meter
- Continuous glucose monitors (CGMs)
Your healthcare provider will help you determine the ideal blood sugar range for your specific situation.
Oral Medications
For people with Type 2 diabetes, prediabetes, or gestational diabetes who still produce some insulin, oral medications like metformin can help manage blood sugar levels.
Insulin Therapy
People with Type 1 diabetes require synthetic insulin injections to survive and manage their condition. Some individuals with Type 2 diabetes may also need insulin therapy. Insulin can be administered in a few ways!
- Insulin pens
- Insulin pumps
- Rapid-acting inhaled insulin
Diet and Nutrition
What you eat has a significant impact on your blood sugar levels, so meal planning and following a healthy, diabetes-friendly diet is essential. For those on insulin, counting carbohydrates and adjusting insulin doses accordingly is a crucial part of management.
Exercise
Regular physical activity helps increase insulin sensitivity and reduce insulin resistance, making it an important component of diabetes management for everyone with the condition.
Weight Management
Maintaining a healthy weight can help improve insulin sensitivity and reduce the risk of complications.
Blood Pressure and Cholesterol Control
Due to the increased risk of heart disease associated with diabetes, it’s important to keep your blood pressure and cholesterol levels within healthy ranges.
Preventing Diabetes
While you can’t prevent autoimmune or genetic forms of diabetes, there are steps you can take to lower your risk of developing prediabetes, Type 2 diabetes, and gestational diabetes!
- Eat a healthy, balanced diet
- Get regular physical activity
- Maintain a healthy weight
- Manage stress effectively
- Limit alcohol consumption
- Get adequate sleep
- Quit smoking
- Take medications as prescribed
Remember, some risk factors like genetics, age, and race are out of your control, but making lifestyle changes can still have a significant impact on your overall risk.

When to See a Healthcare Provider
If you haven’t been diagnosed with diabetes but are experiencing symptoms like increased thirst, frequent urination, fatigue, or blurred vision, it’s crucial to see a healthcare provider right away.
If you’ve already been diagnosed with diabetes, regular check-ups with your diabetes care team (which may include an endocrinologist) are essential for monitoring your condition and making any necessary adjustments to your treatment plan.

A Note from Primary Care Centers of Texas
Living with diabetes can be a challenging journey, but it’s one that you don’t have to navigate alone. At Primary Care Centers of Texas, we understand the complexities of this condition and are here to support you every step of the way.
Our team of compassionate healthcare professionals is dedicated to providing you with the knowledge, tools, and personalized care you need to manage your diabetes effectively. We believe in empowering you with the information and resources to take an active role in your health and well-being.